Insider Brief
- Artificial intelligence is transforming cancer detection, diagnosis, and treatment, offering improved precision, efficiency, and personalized care.
- A study in Nature Cancer by NIH researchers categorizes AI’s impact into ten key hallmarks across screening, diagnosis, treatment optimization, and drug discovery.
- Despite AI’s potential, challenges remain in data standardization, regulatory approval, and bias mitigation, necessitating collaboration among scientists, clinicians, industry, and regulators.
Artificial intelligence is changing how doctors detect, diagnose, and treat cancer, offering new tools to improve survival rates and develop targeted therapies. A recent study in Nature Cancer outlines ten key ways AI is advancing precision oncology, from early screening to drug discovery.
In the study, the team of National Institutes of Health researchers outline the major AI model types and input data modalities and synthesize the latest AI achievements into three broad categories, encompassing ten hallmarks. They also undertook a survey of interventional clinical trials that have incorporated AI.
According to the researchers, cancer remains one of the deadliest diseases worldwide, with cases expected to rise to 28.4 million by 2040. Traditional treatments are often based on broad categories rather than individual patient profiles, limiting effectiveness. AI is helping to change that by analyzing vast amounts of medical data to make cancer care more personalized and efficient.
The researchers point out some of the ways AI is helping oncologists:
AI in Cancer Prevention and Diagnosis
1. Smarter Cancer Screening
AI-powered screening tools are improving the early detection of cancers such as breast, lung, and colorectal. Unlike conventional methods, AI can analyze large sets of medical images and patient histories to spot subtle warning signs. Deep learning models trained on mammograms can flag suspicious findings with higher accuracy than human radiologists, potentially reducing false positives and unnecessary biopsies.
AI also enhances risk prediction, analyzing lifestyle, genetics, and medical history to determine personalized screening schedules. For example, models predicting lung cancer risk based on smoking history and CT scans have demonstrated superior accuracy to traditional methods.
2. Improved Cancer Detection
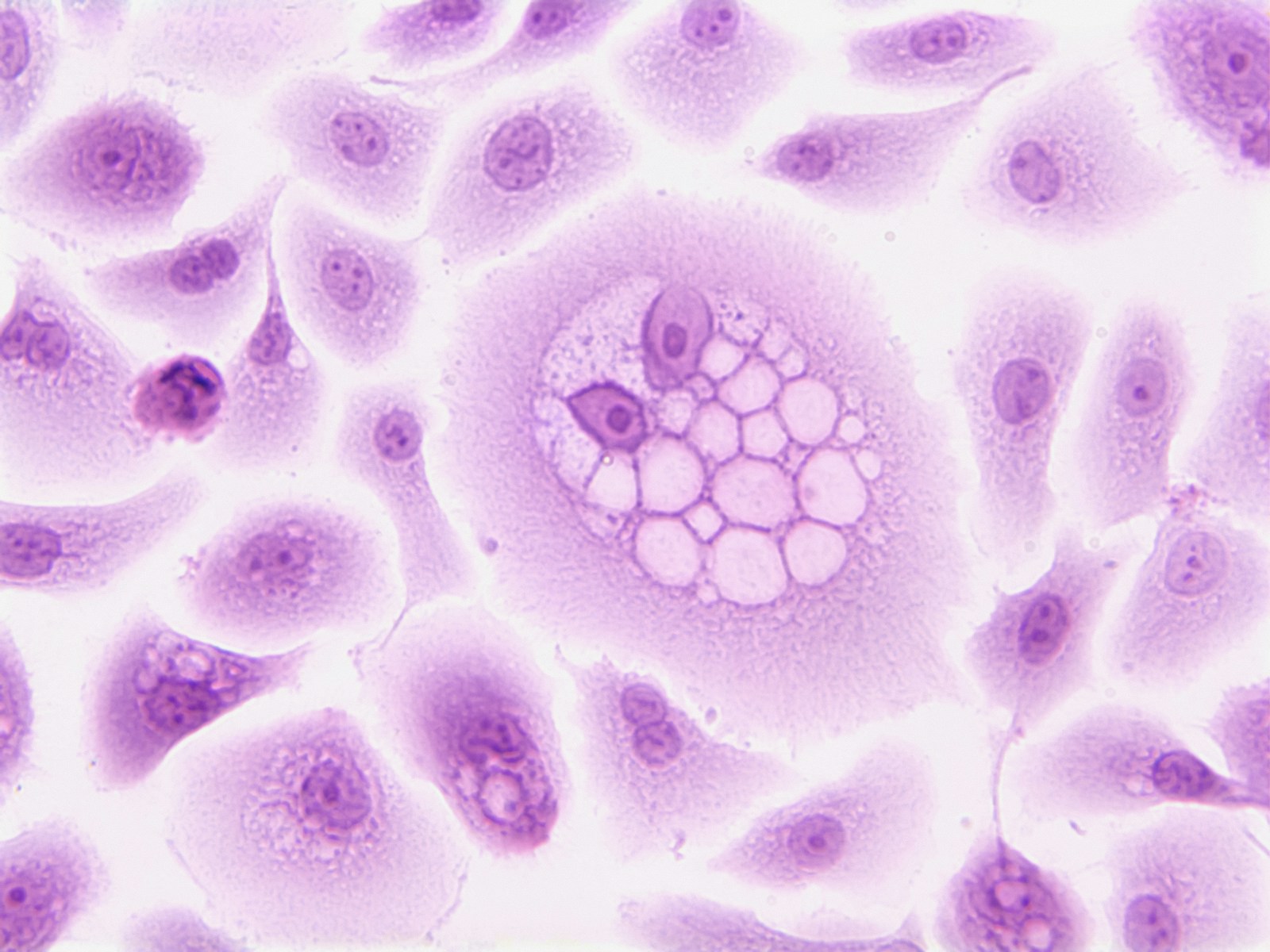
Once a patient has symptoms or a suspicious screening result, AI can assist in confirming a cancer diagnosis. Machine learning models analyze biopsy slides, imaging scans, and even blood tests to identify cancerous cells with high precision.
AI-powered pathology tools reduce the workload on human specialists while improving speed and accuracy. Some AI tools can match or outperform human pathologists in detecting tumors, especially in hard-to-diagnose cases like pancreatic or brain cancer.
3. Detailed Cancer Profiling
After a diagnosis, understanding the exact nature of the cancer is critical for selecting the best treatment. AI can analyze genetic data, pathology images, and molecular markers to classify tumors more precisely than traditional methods. AI-driven models trained on thousands of digital pathology slides can detect molecular characteristics of tumors that might be invisible to the human eye.
Some models have already been approved for clinical use, assisting oncologists in matching patients with personalized treatment options.
AI in Optimizing Cancer Treatment
4. Predicting Patient Outcomes
AI models can forecast how a patient’s cancer will progress based on historical data from thousands of similar cases. These predictions help doctors weigh treatment options, balancing effectiveness with potential side effects.
For example, machine learning algorithms can predict the likelihood of recurrence in breast cancer patients, allowing for earlier interventions. AI models trained on real-world patient data also estimate survival probabilities based on treatment choices, genetic factors, and tumor characteristics.
5. Optimizing Treatment Plans
AI is also being used to personalize radiation and chemotherapy treatments. In radiation therapy, machine learning models determine the optimal dose distribution, reducing damage to healthy tissue. AI-assisted planning has cut radiation treatment preparation times from days to hours while maintaining accuracy.
AI also supports adaptive treatment strategies, dynamically adjusting therapy based on a patient’s response. This is particularly useful in immunotherapy, where AI helps determine whether a patient is responding or if adjustments are needed.
6. Smarter Clinical Trial Matching
Finding the right clinical trial for a cancer patient can be complex. AI helps by scanning patient records to match individuals with trials based on their specific cancer type, genetic markers, and treatment history. This not only speeds up the process but also improves trial enrollment rates, which are often low due to logistical challenges.
Large language models are increasingly used to interpret complex eligibility criteria in unstructured medical records, further streamlining the clinical trial process.
7. Identifying Treatment Response Biomarkers
AI can pinpoint biological markers that predict how a patient will respond to specific drugs. For instance, machine learning models trained on genomic data have helped identify which melanoma patients are most likely to benefit from immunotherapy, sparing others from ineffective and costly treatments.
In breast cancer, AI has identified genetic and molecular signatures that predict response to chemotherapy, improving treatment selection and reducing unnecessary toxicity.
AI in Advancing New Cancer Treatments
8. Discovering Drug Combinations
Many cancers develop resistance to single-drug treatments, making combination therapies critical. AI models can analyze massive datasets to find effective drug pairings that might not be obvious through traditional research. AI-driven simulations have successfully identified new drug combinations that show promise in early-stage trials.
One AI system analyzed over a million drug interactions and proposed novel combinations for leukemia treatment, which are now being tested in clinical trials. AI is also used to optimize drug sequencing—determining the order in which drugs should be given to maximize effectiveness.
9. Uncovering Cancer Vulnerabilities
AI is helping researchers find weak points in cancer cells that can be targeted with new treatments. By analyzing genetic and molecular data, AI can identify previously unknown pathways that cancer cells rely on for survival, opening the door to new drug targets.
AI-assisted studies have led to the discovery of novel therapeutic targets in glioblastoma, a particularly aggressive brain cancer. These findings are being explored in drug development programs.
10. AI-Powered Drug Discovery
The process of developing new cancer drugs is slow and expensive. AI is accelerating this by screening millions of potential drug compounds and predicting their effectiveness before lab testing even begins. One AI system developed a promising cancer drug candidate in just weeks, a process that traditionally takes years.
AI is also revolutionizing precision drug design by predicting how molecules interact with cancer proteins. The latest AI models, such as AlphaFold, are helping scientists understand protein structures at an unprecedented scale, leading to more effective drug design.
Using AI For Patient Benefit Will Require Extensive Collaborations
For AI to deliver its full potential, these stakeholders must work together to refine models, ensure equitable access, and integrate AI solutions into healthcare in a way that prioritizes patient benefit, according to researchers. This requires transparent validation, robust clinical trials, and ongoing monitoring to assess AI’s real-world impact.
The successful integration of AI in cancer care requires collaboration among key stakeholders, including scientists, clinicians, patients, industry, insurers, and regulators. The team offers several ways these groups could work together on leveraging AI against cancer:
- Scientists develop AI models and ensure their proper implementation in clinical settings. They work on refining algorithms, addressing biases, and improving model interpretability to gain trust from healthcare professionals and patients.
- Clinicians play a critical role by identifying real-world medical challenges AI can address. They evaluate AI tools, provide feedback, and help integrate these solutions into hospital workflows.
- Patients are the most affected by AI-driven innovations. Their willingness to engage with AI-assisted healthcare tools, share medical data, and participate in clinical trials helps drive progress.
- Industry is at the forefront of commercializing AI technology, improving accessibility through user-friendly applications, and developing AI-driven drug discovery platforms.
- Insurers influence AI adoption by determining coverage for AI-driven diagnostics and treatments. Their involvement is essential in evaluating cost-effectiveness and ensuring broad accessibility.
- Regulators such as the FDA and the European Medicines Agency oversee AI deployment in healthcare. They establish guidelines for validation, patient safety, and ethical considerations to ensure AI models meet clinical standards.
Challenges and the Road Ahead
Despite these advances, AI adoption in oncology faces hurdles. Many AI models rely on high-quality, standardized data, which is often lacking. Bias in AI training data can also lead to disparities in accuracy across different patient groups. Moreover, regulatory approval for AI-driven medical tools remains a slow process.
Ethical concerns around AI in healthcare include transparency, patient privacy, and data security. Many AI models operate as ‘black boxes,’ meaning clinicians cannot always explain why a model made a particular recommendation. Efforts are underway to develop more interpretable AI systems that build trust among doctors and patients.
Still, AI is already making a tangible impact, the researchers report. Nearly 1,000 AI-based tools have received FDA clearance for use in oncology, and ongoing clinical trials are testing AI-driven approaches in real-world settings. As AI technology continues to evolve, its role in cancer care is expected to grow, making precision oncology more effective and accessible.
The research team included Tian-Gen Chang, Seongyong Park, Alejandro A. Schäffer, Peng Jiang & Eytan Ruppin, all of the National Institutes of Health.